Blog Post
Current Gene Therapy Landscape: Overview, Challenges, and Benefits
January 3, 2020
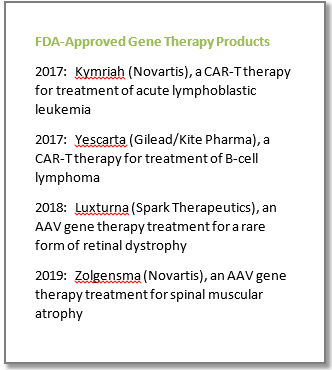
In 2017, the US Food and Drug Administration (FDA) approved its first gene therapy, a chimeric antigen receptor T-cell (CAR-T) product to fight acute lymphoblastic leukemia (Kymriah). That same year, another CAR-T therapy was approved to fight certain types of B-cell lymphoma (Yescarta). Since then, 4 additional products have been approved to treat serious diseases such as B-thalassemia, spinal muscular atrophy, a rare form of vision loss and a rare form of primary immunodeficiency. There are currently over 450 gene therapy and gene-based medicine companies worldwide and around 800 gene therapy and gene-modified cell therapy clinical trials being conducted (ARM Q3 update).
Significant progress has been made in developing safe gene therapy products in recent years. Just over 20 years ago, the tragic case of 19-year old Jesse Gelsinger who died during a gene therapy trial led to a temporary collapse in the gene therapy field. Since then, the gene therapy industry has come a long way. In a joint statement made in January 2019, FDA Commissioner Scott Gottlieb and CBER Director Peter Marks noted that based on an assessment of the current pipeline and clinical success rates of gene therapy products, the FDA anticipates that by 2020 they will be receiving more than 200 INDs per year for cell-based or directly administered gene therapies and by 2025 the FDA will be approving 10 to 20 cell and gene therapy products a year.
The basics – what is gene therapy?
Gene mutations can be inherited or occur as cells age or become exposed to certain chemicals. Small changes to our genetic material can have large impacts on cellular function.
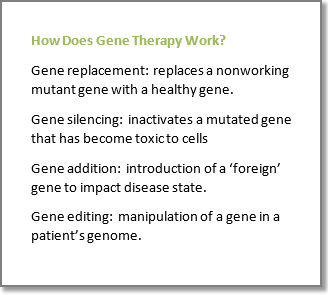
Gene therapy products mediate their effect by transfer of genes or alteration of human genetic sequences. It can be thought of as the introduction, removal, or change of genetic material within patient cells – for instance, repairing a faulty gene in order to produce new or modified proteins, increase proteins that will fight disease, or reduce proteins that cause disease. This can be achieved by gene replacement, gene silencing, gene addition, or gene editing.
The genetic material is typically transferred into patient cells using a specific type of delivery mechanism (described below). Once inside the cell, the gene will make functional protein or target the disease-causing gene.
Gene Delivery Mechanisms
Gene therapy administration can occur via ex vivo or in vivo mechanisms. With ex vivo gene therapy, targeted cells (eg, chimeric antigen receptors (CAR) T cell therapies, T cell receptor (TCR) therapies) are extracted from the patient and the cells are genetically modified in vitro before they are transferred back into the patient. In vivo administration occurs via direct delivery to the patient using a viral or non-viral vector and the target cells remain in the body of the patient.
Vectors (carriers of the gene), can come in the form of viral vectors, which are genetically engineered viruses that replace the virus genome with the therapeutic gene. Examples of viral vectors are retroviruses, lentiviruses, and adeno-associated virus (AAV; of note, the AAV method is believed by many to be the future of gene therapy). Plasmids (small DNA circles or “naked” DNA), engineered bacteria, and liposomes are other vectors of gene therapy administration to either carry and deliver a replacement gene or to help or silence an existing gene.
Another type of gene therapy product is genome edited cells, which can be generated using zinc finger nucleases (ZFNs); transcription activator-like effector-based nucleases (TALEN), or nucleases such as Cas9 and Cas12a that derive from the Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR/Cas). For instance, one company is using a genome editing platform called ARCUS derived from a natural genome editing enzyme called a homing endonuclease in their CAR-T development programs.
Challenges and Benefits in Developing Gene Therapies
The unique benefits of gene therapy are that it targets the cause of the disease and has the ability to treat or maybe even cure rare, debilitating diseases that have few to no treatment options, often with a single administration. Over time, the high price tag of gene therapy could reduce or eliminate the need for a lifetime of expensive and/or painful ongoing treatments that many in this patient population would require.
Although gene therapy offers a number of unique benefits, a number of challenges exist that make the development of gene therapies difficult as well as expensive. Those include:
• Length of clinical trial process – long term safety follow up due to uncertainty surrounding the potential durability of effect and long-term safety effects or complications;
• Manufacturing is complex and time intensive, and many sponsors have faced capacity constraints due to the difficulty in mass production (of viral particles, for instance);
• Individual response variability;
• Some conditions have many mutations leading to a given disease and one gene therapy approach may only work for a subset of affected individuals;
• May stabilize disease pathology but not actually reverse existing damage;
• The efficiency of gene transfer with vectors and the limited control over where integrating viral vectors will integrate;
• Dose of vectors may be high and large doses may be needed to reach target tissues; vectors could be filtered out in the liver or cleared by an immune response;
• Unlike other therapeutics, once administered there is no dose titration and no ability to control expression levels; gene therapy cannot be turned on or off. It is also very likely that there is no ability to do repeat dosing due to immunity developed during initial treatment.
An Advancing Field
Gene therapy offers the potential for significant breakthroughs and a lot of exciting progress has been made with scientific advances in gene therapy and the recent FDA approvals. Their complexity to develop should not be underestimated, as evidenced by the FDA’s release of 6 additional guidances in 2018 intended to help product developers. The gene therapy industry is poised for the future, but due to its complexity the development process needs to be thoughtfully planned and managed. Critical to the success of the field will be the capacity to scale up for AAV manufacturing or other gene therapy manufacturing factories and a streamlined regulatory landscape.
Rho Can Help
There are several unique aspects of gene therapy clinical trials. Rho is currently leading several gene therapy studies and has conducted over 20 gene/cellular therapy trials in over 1000 patients. One of our sponsors commented, “Our collaborative relationship with Rho has been instrumental in the implementation of a complex and rigorous first in human genetic medicine study, including strategic solutions for unique challenges faced in rare disease gene therapy trials. Rho has leveraged existing relationships with patient advocacy organizations and worked closely with a centralized biosafety review partner early in study startup to help identify and mitigate potential challenges. “
From both a clinical and regulatory standpoint, our experts can offer advice on your gene therapy trial from the preclinical phase through post-submission. For additional gene therapy considerations from our experts, please view our webinar, “Development Advice for Gene Therapy Products” and for regulatory considerations, David Shoemaker’s article, “The Gene Therapy Product Development Process.”
Need support designing and executing your next gene therapy trial? Ask our experts for help.
 Kristin Gabor, PhD, RAC, Research Scientist, has experience in both regulatory submissions and clinical operations management, with over 10 years of experience in scientific writing and editing clinical and nonclinical documents, which includes numerous publications in peer-reviewed scientific journals. Dr. Gabor has led and participated in the authoring, review, and preparation of several regulatory and clinical documents, including protocols, clinical study reports, annual safety reports, modules of regulatory submissions (NDA, IND, etc.), and other regulatory documents in a variety of therapeutic areas at various stages of integrated product development programs. Her experience spans a spectrum of therapeutic areas, including cystic fibrosis, sickle cell disease, inflammation and immunology, infectious diseases, atopic dermatitis, multiple sclerosis, and rare diseases. Dr. Gabor earned an interdisciplinary PhD in Functional Genomics from the University of Maine and subsequently received an Intramural Research Training award from the NIH/NIEHS for her postdoctoral studies investigating the role of cholesterol metabolism and cell membrane perturbations in regulating the innate immune response in a rare genetic disease. Dr. Gabor received her Regulatory Affairs Certification from the Regulatory Affairs Professionals Society (RAPS) in 2018 and is a current member of RAPS and the North Carolina Regulatory Affairs Forum (NCRAF).
Kristin Gabor, PhD, RAC, Research Scientist, has experience in both regulatory submissions and clinical operations management, with over 10 years of experience in scientific writing and editing clinical and nonclinical documents, which includes numerous publications in peer-reviewed scientific journals. Dr. Gabor has led and participated in the authoring, review, and preparation of several regulatory and clinical documents, including protocols, clinical study reports, annual safety reports, modules of regulatory submissions (NDA, IND, etc.), and other regulatory documents in a variety of therapeutic areas at various stages of integrated product development programs. Her experience spans a spectrum of therapeutic areas, including cystic fibrosis, sickle cell disease, inflammation and immunology, infectious diseases, atopic dermatitis, multiple sclerosis, and rare diseases. Dr. Gabor earned an interdisciplinary PhD in Functional Genomics from the University of Maine and subsequently received an Intramural Research Training award from the NIH/NIEHS for her postdoctoral studies investigating the role of cholesterol metabolism and cell membrane perturbations in regulating the innate immune response in a rare genetic disease. Dr. Gabor received her Regulatory Affairs Certification from the Regulatory Affairs Professionals Society (RAPS) in 2018 and is a current member of RAPS and the North Carolina Regulatory Affairs Forum (NCRAF).